Gluteal Tendinopathy
 Do you have pain on the side of your hip?
Do you have pain on the side of your hip?
One of the most common sources of side hip pain is gluteal tendinopathy. The pain is usually located around your gluteal muscle tendons and bursa, aggravated with certain physical movements (walking and doing steps) and in certain positions. This blog post will give you an idea of what is going on and what you should do to manage the condition.
What is Gluteal Tendinopathy?
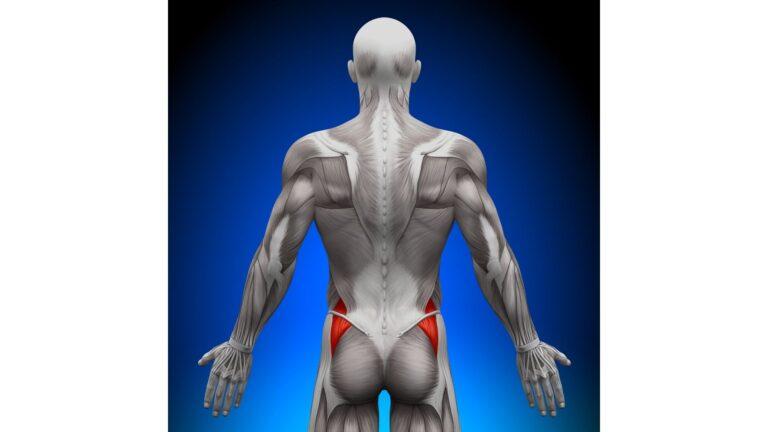
Gluteal Tendinopathy, also known as lateral hip pain, is a condition presented with pain and tenderness around the side of your hip (see below image). Some of the symptoms include localised side hip pain at night with side lying and pain on standing/walking/going up stairs. These symptoms are often associated with gluteal/hip bursitis, but they are not the same thing. The condition is more common in mid-life athletes and the non-physically active population; females also have a higher risk of developing this condition due to the anatomical design of the pelvis and hip.
Gluteal means your bottom area. And tendinopathy means the tendon is overloaded and injured, and therefore unable to heal normally. Usually, tendinopathy is due to overuse over a period of time; therefore it is quite common for tendinopathy to progress into a chronic condition.
Why do the tendons become overloaded?
There are multiple causes of a tendon overload. Some examples include:
- Increase in daily activities – a recent change in walking distance, exercise routine/intensity and step count can influence your tendon load. Sometimes the tendon is unable to adapt to the change which can lead to pain.
- Change of lifestyle/environment – which could be as simple as sitting with your leg crossed when you don’t normally, or changing to a new firmer-than-usual mattress. Compression around the area can influence the tendon load and possibly irritate the area.
- Change of lifestyle/environment – which could be as simple as sitting with your leg crossed when you don’t normally, or changing to a new firmer-than-usual mattress. Compression around the area can influence the tendon load and possibly irritate the area.
What can I do?
It is usually easier to resolve pain and dysfunction during the early stage of the condition. The best way to avoid long term pain is to see your physiotherapist early, as tendinopathy can often be difficult to resolve once it becomes long term. Getting early assessment and treatment can minimise your pain intensity and episodes, and can also help you to return to your normal activities more quickly.
Once your physiotherapist has thoroughly assessed your hip, they will perform treatments and suggest a few lifestyle adjustments to break your pain cycle and start your rehabilitation process. Manual therapy, ultrasound and ice packs can be useful for pain management, but our goal is to slowly strengthen the tendon without causing excessive pain. Exercise remains the most important and effective way to help with managing tendon pain.
We will likely prescribe simple and easy exercises initially to activate muscles and tendons. Once the pain is mostly under control, we will keep progressing the exercises to further improve strength and resilience of the underlying structures. We will also encourage general lower body exercise to improve your lower limb strength and movement pattern. Once you are pain free, we will work with you to ensure the pain doesn’t come back and keep your body strong with ongoing exercise.
Doctor or medical scan said I have gluteal bursitis. Is that the same thing?
Gluteal tendinopathy and bursitis are both under the category of lateral hip pain. Bursitis means the bursa is inflamed. Bursa is a fluid sac between your tendon and bone, like a cushion. It is designed to reduce friction and irritation between structures. Research has shown that tendinopathy is usually the primary cause of lateral hip pain, and bursitis is likely secondary.
Chronic bursitis/tendinopathy requires both time and exercise to slowly reduce pain and improve function. Treatment will be similar for both conditions. If the bursitis is from a trauma or massive overload event (e.g., a fall), then the management will be slightly different. See your physiotherapist for an assessment and management plan to suit your specific needs.



